If the pressure in the portal vein becomes too high (mostly as a result of liver diseases, like alcohol cirrhosis) pressure builds in the connecting vessels too. Veins have thinner walls than arteries and tend to balloon under pressure.
As a result, the normally small veins around the navel dilate in size and become visible beneath the skin, fanning in all directions. This sign, like a head replete with snakes for hair, is named caput medusae, or Medusa’s head. In Greek mythology, the gorgon Medusa whose head was severed by the hero Perseus, had the ability to turn anyone who beheld her gaze to stone.
And on that topic, all that dirt, debris and dead skin in our navels should also get an honorable (or maybe dishonorable) mention—prolonged accumulation of this material within the cavity can make it harden over time, forming a stony mass. We call this an omphalolith, or umbilical stone.
So the umbilicus is something of a reliable crystal ball in diagnosing internal illnesses. But as to whether you regard it as an attractive part of your own anatomy, one has to ask the question: are you innie or outie?
An alternative method of transferring blood cells to weakened newborns through their umbilical cord does not carry long-term neurodevelopmental risks compared to standard practice, a recent study found. The research will be presented at the Pediatric Academic Societies (PAS) 2024 Meeting, held May 2–6 in Toronto.
By examining lipid rafts in rat models, the researchers found an increase in the percentage of a protein called L1 cell adhesion molecule. This increase was found in both sides of the brain cerebellum. The cerebellum plays a large role in developing motor, cognitive and emotional functions in babies.
“The proportion of the protein in lipid rafts increased by seven-fold in some cases. These changes persisted after hypothermia,” said Bearer, who is also the William and Lois Briggs Chair in Neonatology. “The same increase in the proportion of L1 protein in lipid rafts occurred even when the research models were not treated by hypothermia, which shows hypothermia did not reverse this effect of HIE.”
Bearer said their findings show that hypothermia alone is not an effective treatment for reversing the effects of HIE and supports the team’s rationale that lipid rafts may be a target for more effective treatment.
For example, the researchers say one possible intervention strategy worth further study could be dietary, specifically focusing on a nutrient called choline. Choline is found in some foods, especially egg yolks, and plays a key role in brain development and lipid rafts.
“This study is the first of its kind to look at lipid rafts and their involvement in HIE,” Bearer said. “I am encouraged that these results will lead to more effective interventions to prevent brain injury.”
Very premature babies need extra oxygen and mechanical intervention to breathe, but this damages their lungs, causing a chronic lung disease called bronchopulmonary dysplasia (BPD). These babies have smaller and weaker lungs that can’t send as much oxygen to their growing brains. The lack of oxygen during brain development can lead to learning disabilities, or problems walking, hearing and seeing.
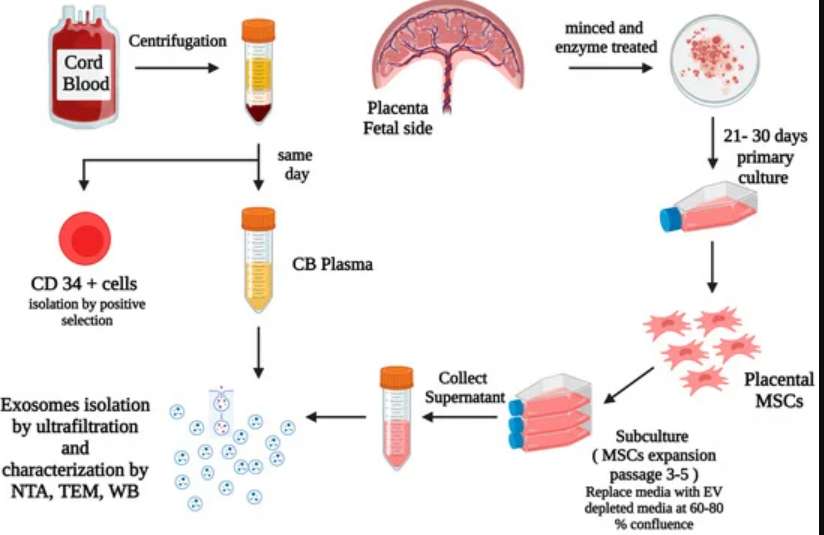
There is no cure for BPD, but Dr. Bernard Thébaud and his team are hoping to change that. The team previously found that cells from the umbilical cord, called mesenchymal stromal cells or MSCs, could prevent BPD in newborn rats.
The team is now partnering with Stanford University to implement their test in several other countries. They are also exploring the use of artificial intelligence to make it even better.
RUDN researchers have proposed freezing parts of human umbilical cord, among other things, to obtain stem cells. Unlike conserved umbilical blood, the perivascular tissue of the umbilical cord (Wharton’s jelly) is an effective and safe source of mesenchymal stem cells. An article describing the results of the work was published in Stem Cell Research & Therapy.
After a baby is born, the umbilical blood is preserved in the afterbirth and the umbilical cord. It contains hematopoietic stem cells that can be used to treat leucosis, lymphoma and complicated cases of anaemia. Within the previous decade, scientists also discovered useful properties of other umbilical cord tissues, especially the vessels of the cord and the Wharton’s jelly—mucilaginous material that fills the umbilical cord, makes it flexible, and prevents the vessels inside it from clotting. For further medical use, these tissues undergo cryoconservation, i.e. are stored in liquid nitrogen at -196℃. Cryoconservation stops all chemical processes in cells, and after they are defrosted, their biological functions restore.
“Storing umbilical blood is a popular procedure all over the world. However, besides it one may also store cells from Wharton’s jelly and the tissues of the umbilical cord itself. It is virtually a source of fetal cells, but their use is not associated with any ethical or legal issues. We suggest freezing parts of the umbilical cord tissue and then defrosting them and using to generate cell cultures,” says Timur Fatkhudinov, a co-author of the work, and a professor of the Department of Histology, Cytology, and Embryology of the Institute of Medicine, RUDN.
The cryoconservation of the umbilical cord is 2.5 times cheaper than of the umbilical blood. However, RUDN researchers believe umbilical blood as a source of hematopoietic stem cells (blood cell precursors) and other umbilical cord tissues (sources of mesenchymal stem cells, an effective tool of regenerative medicine) should be frozen separately.