The new findings suggest that concerns raised by a 2019 study of infants born before 28 weeks—which concluded that umbilical cord milking might increase the risk of bleeding inside the brain—do not apply to preterm infants born after 28 weeks. The current study appears in Pediatrics.
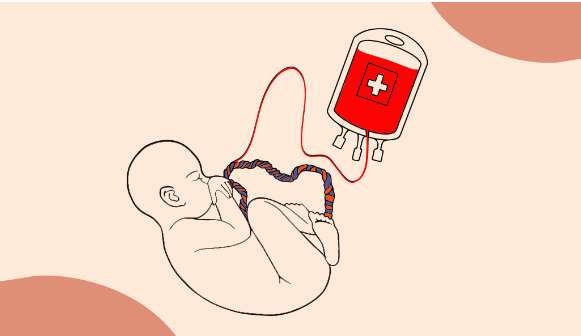
The standard procedure, delaying cord clamping while blood naturally flows into the infant’s body, takes 30 to 180 seconds. However, cord milking, takes about 20 seconds, reducing delay for infants who need immediate assistance, such as respiratory support. Both procedures allow for umbilical cord blood to reach the infant’s body before clamping, reducing the risk of anemia and other complications seen among infants receiving immediate cord clamping and cutting.
The study was conducted by Anup Katheria, M.D., of the Sharp Mary Birch Hospital for Women & Newborns in San Diego, and colleagues in the United States, Canada and Europe.
“We need more research to confirm these findings and to understand more about the links between exposure to heavy metals in the womb and children’s health in the longer term.”
Professor Annesi-Maesano and her team continue to study heavy metals and other environmental pollutants and their effects on asthma and allergies.
Daiana Stolz, who was not involved in the research, is the European Respiratory Society (ERS) Education Council Chair and is Professor of Respiratory Medicine and a leading physician at the University Hospital Basel, Switzerland. She said: “We know that heavy metals that are present in many everyday products can be damaging to health if they enter our bodies through the air we breathe, or our food and drink. It’s particularly worrying to know that cadmium and other metals might be reaching unborn babies via the umbilical cord.
“We need to understand the possible causes of asthma and allergies in children so we can try prevent these conditions. This research indicates that higher levels of cadmium in cord blood could have an influence on children’s risk of asthma and allergies, but it’s a small study, so we do need to keep investigating this issue.
“Given the known dangers of cadmium and other heavy metals, this study supports extremely tight regulation of their use and careful disposal of products, such as batteries, that contain cadmium.”
Researchers at UPMC Children’s Hospital of Pittsburgh found that infusing umbilical cord blood—a readily available source of stem cells—safely and effectively treated 44 children born with various non-cancerous genetic disorders, including sickle cell, thalassemia, Hunter syndrome, Krabbe disease, metachromatic leukodystrophy (MLD) and an array of immune deficiencies. This is the largest trial of its kind to date.
Improving the tools that measure an infant’s diabetes exposure—and relevant protein fluctuations—at the time of birth “would increase the accuracy of health assessments to enable more informed predictions of long-term health outcomes,” the researchers wrote. “Unfortunately, these [conditions] often go undiagnosed until children present with disease later in life, at which time the opportunity for prevention has ended.”
In a 10-patient cohort study led by Dr. Jean Roy, hematologist and professor at the Faculty of Medicine of Université de Montréal, that aims to understand how to mitigate the risks associated with the treatment of multiple myeloma, a malignant cancer, researchers have adopted an innovative approach based on the unique immunological properties of umbilical cord blood in an effort to improve the safety and efficiency of allografting, the preferred treatment for this disease.
“This step forward has given new hope to those struck by this terrible disease,” said Dr. Denis-Claude Roy, Director of Research at the CIUSSS de l”Est-de-l’Île-de-Montréal (CIUSSS-EMTL).
This work, conducted at Hôpital Maisonneuve-Rosemont, is funded by the Canadian Stem Cell Network, the Maryse and William Brock Chair for applied research in stem cell transplantation of Université de Montréal, and the biotechnology company ExCellThera.
The challenge of allografting
Multiple myeloma, one of the most common bone marrow cancers in Canada, is still incurable, and those afflicted have a life expectancy of approximately five to six years. Patients who are at an advanced stage of the disease who have chromosomal anomalies, show myeloma cells in their blood, or do not respond to their initial treatment have a reduced life expectancy of approximately three years. Until now, the only possible treatment for patients with multiple myeloma has been stem cell grafting from related or unrelated donors. However, allografting is associated with several side effects, the most significant being graft-versus-host-disease, a condition that arises when the donor cells attack the receiver’s organs. This complication has a 10-to-20 per cent mortality rate. In long-term survivors, immune system complications (up to 80 per cent of patients) and relapses (up to 50 per cent of patients) are still much too frequent. Allografting must therefore be refined to successfully treat a greater number of multiple myeloma patients.